
Disparities in PAD:
A Growing Concern
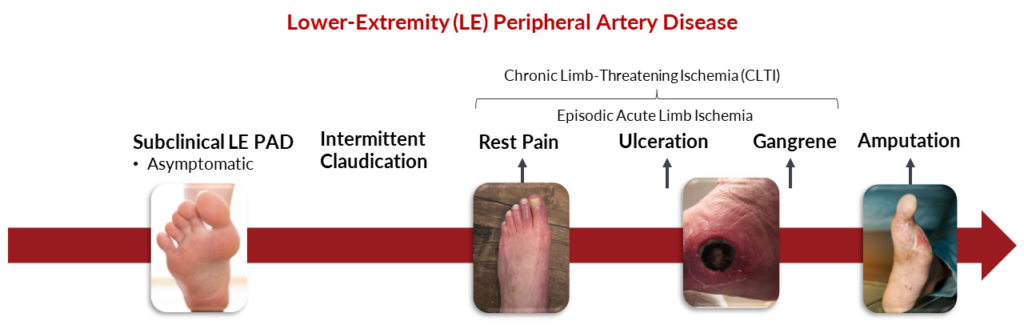
Peripheral Arterial Disease disproportionately affects communities that face economic and social challenges. Key social determinants such as health care access, neighborhood conditions, and education all contribute to disparities in PAD outcomes1. Additionally, certain ethnic groups and women are at higher risks for more severe PAD complications.
Understanding these factors is critical to closing the gap and improving care for those most vulnerable.
Social Determinants of Health (SDoH) and PAD
- Insurance Coverage
- Health Literacy
- Transportation to Health Care Facilities
- Copays
- Provider Availabilities
- Quality of Care
- Housing
- Transportation
- Safety
- Walkability
- Recreation/Parks
- Water Quality
- Access to Healthy Food
- Social + Community Integration
- Support Systems
- Community Engagement
- Stress
- Discrimination
- Employment
- Income
- Debt
- Expenses
- Support
- Medical Bills
- Higher Education
- Literacy
- Early Childhood Education
- Language
- Vocational Training
Ethnic and Gender
Risk Factors in PAD
David Fornell, 5-time winner of the Jesse H. Neal award interviews
Dr. Kumar Madassery (Rush University, Chicago)2
“What we see in Chicago mirrors what we see around the country, in that these healthcare deserts where there is low access to care or detection of disease is only in late stages, are the same areas with the highest amputation rates.” – Kumar Madessery, MD
African American
- 1 in 3 Black American adults may develop PAD compared to Hispanics or White3
- Present with more severe disease
Hispanic/Latino
- Adults with predominantly sedentary lifestyles have a higher risk of PAD, even in the absence of other risk factors4
Women
- 30% more likely to have PAD than men5
- Symptoms or exertional leg pain is absent with >60% of women with PAD6
- Intermittent claudication tends to present 10 – 20 years later than men7

PAD does not affect all populations equally.
Barriers to Early Detection and Treatment
In 2021, the American Medical Group Association (AMGA) conducted a roundtable to explore the barriers to early PAD detection and treatment across diverse communities.8 They engaged with 18 experts from geographically and medically varied backgrounds to understand the systemic challenges facing PAD patients. The findings highlighted the following barriers:
These barriers underscore the importance of healthcare reform and community-based initiatives aimed at improving PAD awareness, accessibility, and care.
Read the full study here: Perspectives on Lower Extremity Peripheral Artery Disease: A Qualitative Study of Early Diagnosis and Treatment and the Impact of Health Disparities

